“When we look at tech, the first question we ask ourselves as a design team and an innovation team is, is this going to make the experience more human or less?”
—Chris Waugh, Chief Innovation Officer at Sutter Health
In our most recent Creative Confidence Series chat, Chris Waugh, Chief Innovation Officer at Sutter Health, and IDEO U Dean Suzanne Gibbs Howard sat down to discuss how service design can radically and rapidly change the ways healthcare is delivered, making it more personalized and a better experience for patients.
In his time in the healthcare space, Chris Waugh has worked with the Centers for Disease Control while at IDEO, as Vice President of Design at One Medical, and now leads innovation efforts at Northern California-based Sutter Health, an organization with 55,000 employees, 3.5 million patients, and every piece of the care continuum, from pediatrics to transplant care. To innovate in this complicated space, he relies on design thinking, putting humans at the center of the process. “For us in healthcare, design is how it all threads together,” Chris says. His team’s goal is to make healthcare simpler, more engaging, more human, and more affordable. “Unlike other brands where you get a sliver of everyone’s life, these are the most meaningful moments of people's lives,” he says with regards to how healthcare plays a role in every stage of our lives.
Prioritizing and Fast-tracking Innovation Efforts
To keep their true north, Chris’s team’s number one metric is lives touched. While their ultimate goal is to reach as many lives as possible, early phase projects need to take less than three months, and reach less than 100 people. Those constraints “keep you from overthinking and it keeps you from perfecting,” he says. With smaller projects, you can be more disruptive and progressive, test for any negative consequences, increase creative confidence, discover if you’re ready for to duplicate it site, and then go full scale.
The other two most important metrics are economic viability and clinical viability. Obviously, positive clinical outcomes are key, but economic viability is also a huge piece of success, even if a project or idea might have philanthropic dollars behind it. “We want your design to live for a lifetime,” he says. “So if we implement this from a position of economic viability, your design is going to make it.”
To drive change at Sutter, the team also relies on an innovation accelerator, a group appointed by the leadership team that includes representatives from Human Resources to Legal and many other departments across the organization. “They see ideas almost as soon as we see them,” he says.
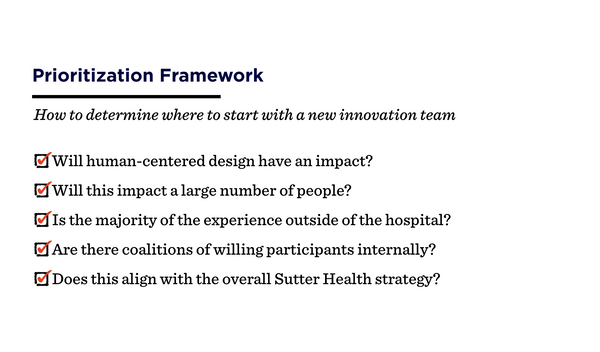
With so many potential design projects to pursue, a simple question framework helps the team prioritize which projects will have the most impact toward their overall goals.
Innovating Everyday Healthcare
To reach their goal and impact the most lives possible, the innovation team at Sutter chose to focus on “everyday health” — ongoing care that most people need. One of the first projects Chris worked on at Sutter dealt with a tough topic—advance directives and end of life care. Planning for death is not something a lot of people want to do, but, as Chris says, “Design can reframe how we want to create this dialogue.” One of the assumptions of end-of-life planning is that people have to be close to death to do it. And often, they don’t do it at all, putting the burden on their loved ones. But what if we had that conversation much earlier in life, as a normal part of primary care? “That’s an interesting example of where design has an immediate impact on one of the toughest decisions on global healthcare,” he says.
In another project aimed at giving those in rural areas the same access to healthcare as those in big cities, Sutter started implementing telecardiology--allowing patients to interact with cardiologists in bigger hospitals remotely from their local healthcare facilities. It removes the hassle tax of asking a patient to drive a long distance--and take even more time off of work--and allows the cardiologists to see more patients. “When we look at a technology, the first question we ask ourselves as a design team and an innovation team is, is this going to make the experience more human or less?”
“What we’re seeing as an innovation team is when it’s all said and done, we will have made health care simpler, more engaging, more human, and more affordable. That’s our true north.”
Chris Waugh
Identifying Collaboration Opportunities Through Journey Mapping
One of the most useful tools in Chris’s arsenal is journey mapping. As he points out, journey mapping is pretty ubiquitous in the business world, but it’s still relatively new in the world of healthcare. The concept is pretty simple: map out the entire patient experience, from their first interaction with the healthcare system to the experience they have that extends beyond the hospital walls well after they receive treatment. “The number one helpful bond of a journey map for us is that everyone can see their part in the experience, including the digital angle of this experience,” he says. “The doctors can see where their magnificent roles are. The nurses can see their roles. The digital [team] can see its role.”

Sutter Health involves a ton of moving pieces, some of which aren’t necessarily the organization’s expertise, like housing for transplant patients or shuttles. In cases where other companies might have a better hold on, say, transportation, the group considers whether a ride-sharing service might be a smarter use of resources than figuring it out themselves. “There is an opportunity where those partners do an extraordinary job of the part of the equation, and it’s a matter of collaborating to create that outcome.”
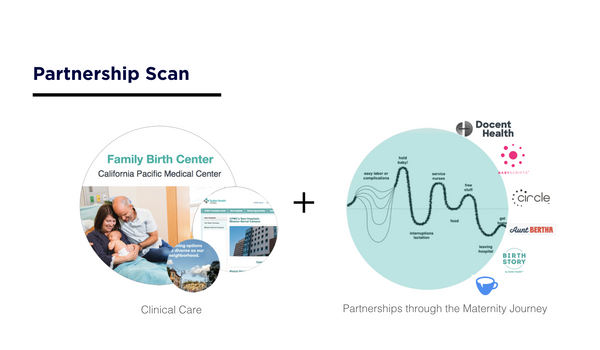
Sutter’s partnership with Lyft showed the value of this collaborative approach. Sutter found that more than 3.6 million Americans miss or delay medical care each year because of transportation issues. By partnering with Lyft on a pilot program to give patients better access to healthcare appointments, they were able to improve the patient experience much faster and better than had they tried to build a solution in-house. In journey mapping the experience for new mothers at Sutter Health, the team found opportunities for partnership after mothers left the hospital.
Creating long-term goal horizons
To keep long-term goals in check, Chris thinks of his team’s work as three different horizons. The third and farthest horizon is the team’s ultimate goal, with nearer horizons as incremental steps toward it.
Think of the first horizon as a smaller experiment--like, for example, providing pregnant women with a docent, someone they can text at all hours for advice. The second is scaling successful new solutions—making docents available by text to all mothers in the system. And the third comes when it’s possible to reduce the number of times new mothers need to go to the doctor while still maintaining a high quality of care for themselves and their baby.
As teams work, it’s important to keep a balance between the three different phases. “You’ve got to throw the ones in there to keep everybody’s confidence up, but you can’t cheat and just do the easy ones and say, ‘See, we’re innovating the whole thing. We’ve touched a million lives by making it just a little better than it was last year.’ That’s not going to work,” he says.
As the innovation team at Sutter looks to the future, they’re continually exploring ways to make the healthcare experience more human. Whether through partnerships or new technology, their purpose remains the same — to augment and enhance the human and caring aspect of the patient experience and touch as many lives as possible.
Interested in learning more about journey mapping and designing innovative experiences? Learn more about our Human-Centered Service Design course.
- choosing a selection results in a full page refresh
- press the space key then arrow keys to make a selection



